DIAGNOSING SPINE PROBLEMS
Before a health care professional can diagnose your condition and design a treatment plan, a complete history and physical examination are necessary. There are so many possible internal causes of pain; it is important to determine what is and is not causing the problem. After the physician has a better idea of what is contributing to your discomfort, diagnostic tests of some sort may be recommended.
HISTORY
First, you will be asked for a complete physical history of your condition. This may begin by filling out a written form that asks you questions relating to your pain. The more information you share with the provider, the easier your problem will be to diagnose. Your physical history is important because it helps your doctor understand when the pain began, anything that could have caused an injury, your lifestyle, physical factors that might be causing the pain, and your family history of similar problems. After reading through your written history, your physician will ask more questions that relate to the information you have given. Some typical questions include:
- When did the pain begin?
- Was there an injury that could be related to the pain?
- Where do you feel the pain? What is the intensity?
- Does the pain radiate to other parts of the body?
- What factors make the pain feel better or worse?
- Have you had an injury or surgery to your back or neck?
- Have you had problems with your bladder or bowels?
- Is there a history of osteoporosis in your family?
Physical Examination
After taking your history, the doctor will give you a physical examination. This allows him or her rule out possible causes of pain and try to determine the source of your problem. The areas of your body that will be examined depend upon where you have pain – for example, in your neck, lower back, arms, or legs. The following are some of the things that are checked in a typical exam:
- Motion of Spine and Neck – Is there pain when you twist, bend, or move? If so, where? Have you lost some flexibility?
- Weakness – Your muscles will be tested for strength. You might be asked to try to push or lift
- your arm, hand, or leg when light resistance is put against them.
- Pain – The doctor may try to determine if you have tenderness of certain areas.
- Sensory Changes – Can you feel certain sensations in specific areas of the feet or hands?
- Reflex Changes – Your tendon reflexes might be tested, such as under the kneecap and under the Achilles tendon on your ankle.
- Motor Skills – You might be asked to do a toe or heel walk.
- Special Signs – The physician will also check for any “red flags” that could indicate something other than spinal/vertebrae problems. Some signs of other problems include tenderness in certain areas, a fever, an abnormal pulse, chronic steroid use (leads to loss of bone mass), or rapid weight loss.
Diagnostic Tests
You may be asked to take a variety of diagnostic tests. The tests are chosen based upon what your physician suspects is the cause of your pain. These are the most common diagnostic tests:
X-RAY
An X-ray is a painless process that uses radioactive materials to take pictures of bone. X-rays can be used to see changes in bone, so they will definitely be used if your doctor thinks you may have a fracture, bone infection, or tumor. During an X-ray, you will be asked to lie very still on a table and hold certain positions while photographs are taken of your spine.
CAT (COMPUTER ASSISTED TOMOGRAPHY) SCAN
The CAT scan is similar to both the MRI and a regular X-ray, because it can show both bones and soft tissues. CAT scans are also able to produce X-ray “slices” taken of the spine, allowing each section to be examined separately. The CAT scan can show disc problems and wear-and-tear of bones, such as a bone spur or enlargement of a facet joint. CAT scan images are not as clear as X-ray or MRI images. To make the soft tissues easier to see, the CAT scan is often combined with a myelogram (my-low-gram).
Like an MRI, with a CAT scan you will lie on a table that slides into a scanner. The scanner is like an X-ray tube that rotates in a circle taking many pictures. The CAT scan procedure takes 30-60 minutes.
MYELOGRAM
A myelogram (my-low-gram) is an older test that is used to examine the spinal canal and spinal cord. This test requires a special X-ray dye to be injected into your spine by a doctor. This is done by inserting a small needle in the lower back and into the spinal canal. When the myelogram is taken, the dye outlines the spinal cord and nerve roots so that disc and bone problems can be seen.
To conduct the myelogram, the patient lies on a tilting table. As the table tilts, X-rays are taken to show the flow of the dye through the spinal region, helping doctors look for problems that may be due to a herniated or bulging disc, lesions, tumors, or injury. The myelogram is often combined with a CAT scan to get a better view of the spine in cross section. In many cases, the MRI has replaced both the myelogram and the CAT scan. Sometimes the myelogram still shows the problem better than the MRI, but today it is used less frequently than the MRI.
BONE SCAN
A bone scan can be used to locate any problem areas of the spine. The bone scan works by injecting a radioactive chemical, sometimes called a “tracer”, into the bloodstream. The chemical will attach itself to areas of bone that are undergoing rapid changes. Over a period of several hours, tracer accumulates in any problem area, making it easier to see with a special camera. Problem areas show up on the film as dark spots or “hotspots”.
A bone scan is very useful when it is unclear exactly where the problem is in the skeleton. The ability to take a picture that lights up the area where the problem seems to be coming from allows the doctor to pinpoint where to look next. After locating the problem areas, other tests can be done to show more aspects of those specific spots. The bone scan can identify problem areas such as bone tumors and compression fractures. A bone scan can also be used to determine bone density and the bone-thinning condition of osteoporosis.
EMG (ELECTRODIAGNOSTIC STUDY)
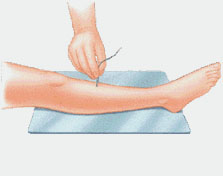
An electromyogram (elec-tro-my-oh-gram) (EMG) is a test that looks at the function of the nerve roots leaving the spine. The test is done by inserting tiny electrodes into the muscles of the lower extremity. By looking for abnormal electrical signals in the muscles, the EMG can show whether a nerve is being irritated or pinched as it leaves the spine.
Think of how you test the wiring on a lamp. If you place a working bulb into the lamp, and the bulb lights up, you assume that the wiring is okay. However, what if the bulb does not light up? You can safely assume that something is probably wrong with the wiring, like the lamp is unplugged, or a short circuit has occurred.
Using the muscles like the light bulb in the lamp, an EMG is able to determine the condition of the nerves that supply those muscles, just like the wiring on the lamp. If the EMG machine finds that the muscles (the light bulb) are not working properly, the doctor can assume that the nerves (the wiring) must be getting pinched somewhere.
SOMATOSENORY EVOKED POTENTIAL (SSEP)
Somatosensory (so-mat-oh-sense-ory) Evoked Potential (SSEP) is a test that shows how well electrical signals travel from your body to your brain. The signals show whether the nerves that connect to your spinal cord are able to send and receive sensory information like pain, temperature, and touch. An SSEP indicates whether your spinal cord or nerves are being pinched. It is helpful in determining how much the nerve is damaged, and whether there is a bone spur, herniated disc, or other source of pressure on your spinal cord or nerve roots.
An SSEP is performed by placing an electrode over the skin or inserting a needle into the nerve or sensory center of the brain. The time it takes for an electrical signal to travel through the nerve pathway is then recorded. The function of the nerve is determined by the speed of the electrical signal. If the nerve pathway is pinched, the signal travels slower than expected.
The SSEP does not show exactly what is causing the problem, only that a problem exists. This is a limitation of the test. However, a positive result does tell your doctor where to look further, which is helpful. Problems detected by an SSEP may not be in the spine itself.
FACET JOINT BLOCK
A facet joint block is a procedure where a local anesthetic medication (such as lidocaine or Novocain) is injected into the facet joint. This same type of medication is used by a dentist to numb your jaw, or a doctor when stitching up a cut. The medication numbs the area around the facet joint. If this causes the pain to go away, the doctor can assume that the facet joint is a problem.
Laboratory Tests
Certain laboratory tests, such as a blood test, may be done to check for problems that are not related to deterioration of the spine. Such tests can help identify such problems as infection, arthritis, cancer, or aneurysm.
SPINAL TAP
A spinal tap is done in order to get a sample of the cerebrospinal fluid that surrounds the spinal cord. The fluid is usually very clear. It contains proteins, sugar, and other substances that can be found in blood. It typically does not contain red blood cells or many white blood cells. A spinal tap checks the pressure and content of the fluid. Signals that there may be problems include: evidence of bleeding, an increase in white blood cells (infection fighting cells, dead cells are “pus”), an increase in protein level, or inflammation. This could mean infection, tumors, or a hemorrhage around the brain or spinal cord. To obtain the fluid sample, a needle will be inserted into the spinal canal in the lumbar region.
DISCOGRAM
A discogram is an X-ray examination of the discs between the vertebrae. This test is used to determine whether a disc is damaged, and whether surgery is necessary. The test is performed by injecting dye into the center of the injured disc. The dye makes the disc clearly visible on X-ray. This test is better than a regular X-ray or a myelogram. The dye helps the doctor make an accurate diagnosis. With a discogram, you will be given medication to help you relax, then a local anesthetic. The procedure usually lasts about 40 minutes.